
Virtual remote appointments are available. Contact us for a video telehealth evaluation.

All appointments conducted by our Board Certified doctor and not assistants or non-physician providers.
What is a spermatocele?

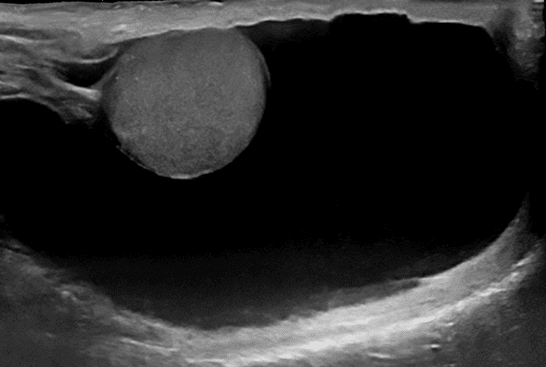
A spermatocele or spermatic cyst is an abnormal sac in the upper part of the epididymis (the epididymis is a coiled tube in the testicle that collects and transports sperm). In most cases, a spermatocele is a smooth, soft mass that contains clear or milky fluid, and sometimes, sperm. The exact reason why spermatoceles develop is unknown but it is believed to be due to a blockage in one or more of the multiple tubes within the epididymis. Spermatoceles are a relatively common problem and are often discovered by chance. Incidental spermatoceles are found in 30% of patients undergoing ultrasound of the scrotum for other complaints.
Why treat a spermatocele?
Spermatoceles are non-cancerous and they do not typically affect fertility. Most spermatoceles are painless. However, a spermatocele can grow large enough to cause discomfort, pain, and a sensation of heaviness or fullness. Spermatoceles are diagnosed by ultrasound which can be done in the office.
Am I a candidate for spermatocele sclerotherapy?
 If the spermatocele becomes large enough to cause a level of discomfort, then treatment maybe recommended. Generally, the spermatocele should be at least 0.5 cm to be amenable to treatment.
If the spermatocele becomes large enough to cause a level of discomfort, then treatment maybe recommended. Generally, the spermatocele should be at least 0.5 cm to be amenable to treatment.
The first step is a diagnosis, which can be done by an ultrasound in the office. Our doctor is a board certified imaging specialist in addition to specializing in minimally invasive procedures and will perform the diagnostic ultrasound during your visit if you have not had one. If you have already had an ultrasound, generally the first step is to have a consultation to understand the procedure, preparation and expected results. Occasionally, the consultation and treatment can be done at the same time.
Our image-guided specialist sees patients throughout the Los Angeles, Orange County and San Diego areas. Contact us today.
Our Patient Experiences
Treatment Options
There are two types of treatments for spermatoceles: sclerotherapy and surgical excision.
Spermatocele Aspiration & Sclerotherapy
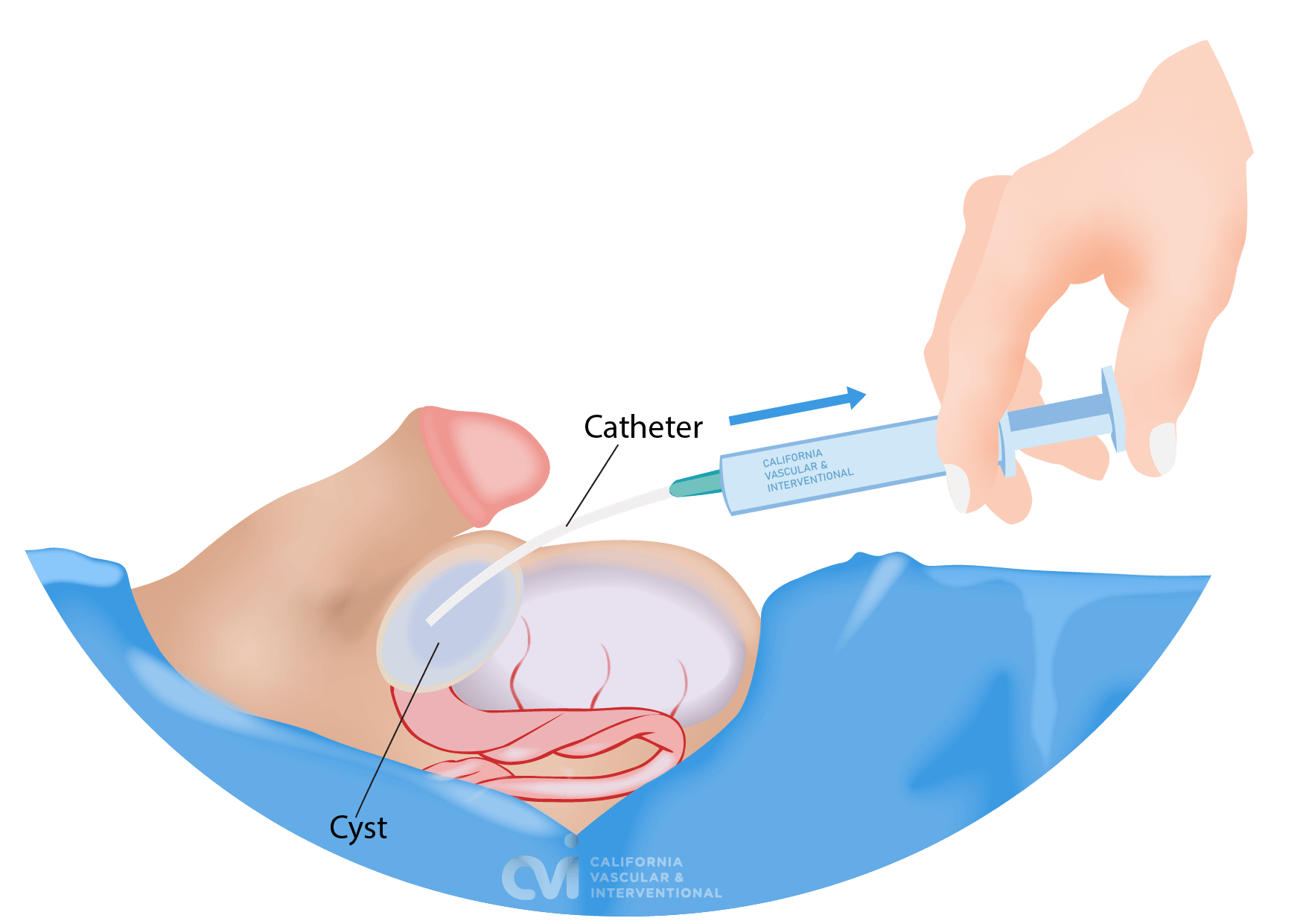
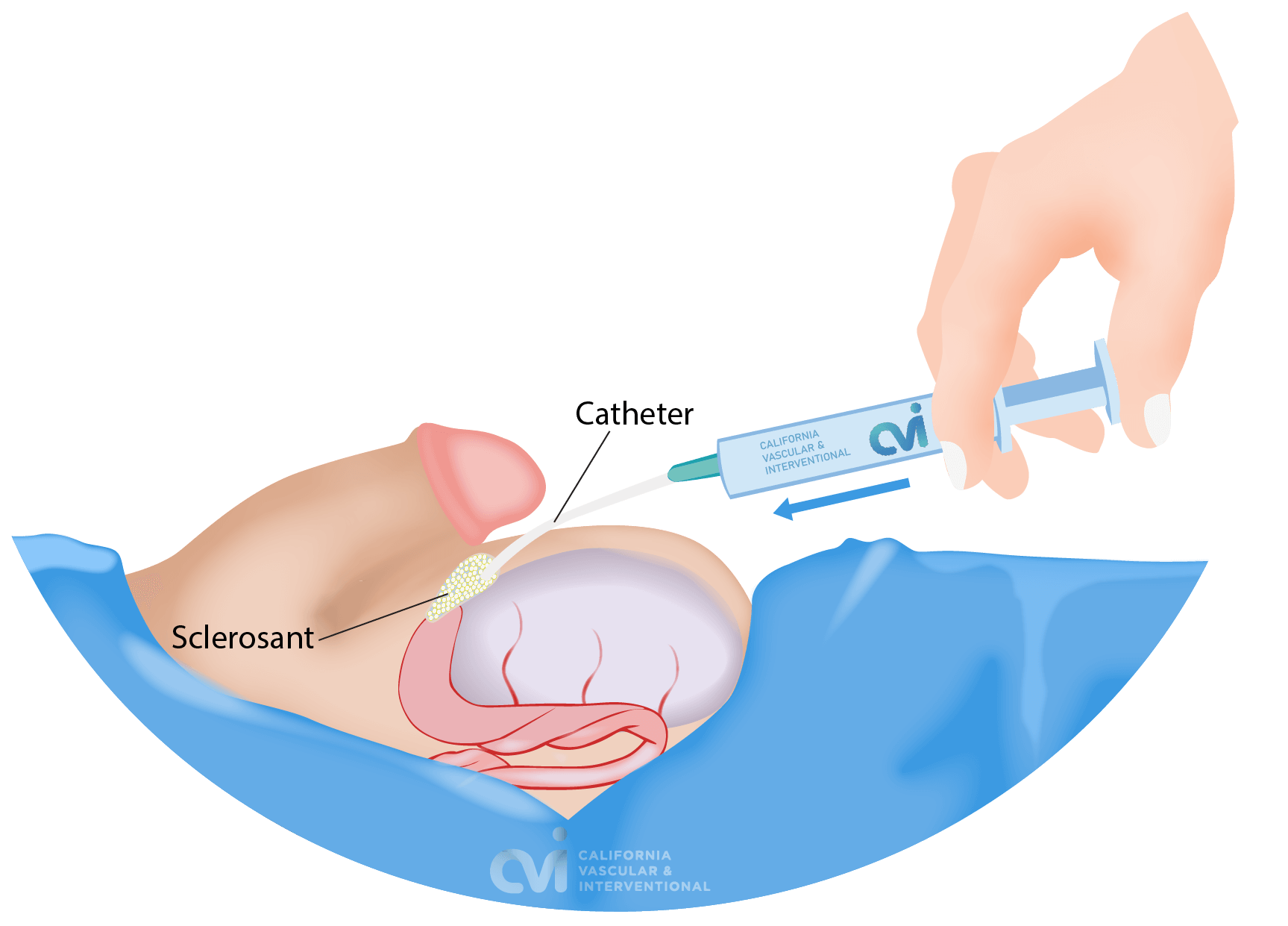
Sclerotherapy is an outpatient procedure performed in the office that involves removing the fluid collection (aspiration) through a small tube followed by injection of a medication (sclerotherapy) that helps close the cavity that was containing the fluid. Our specialist applies a local anesthetic to make the procedure essentially pain-free. There is no downtime, stitches or incisions. You will walk out of the office after the procedure.
This is a minimally invasive, quick, safe, and effective treatment for a spermatocele. The risk of complications is low and patient satisfaction is high.2 Unlike surgical excision, you will not need to wear athletic scrotal support, ice or sutures.
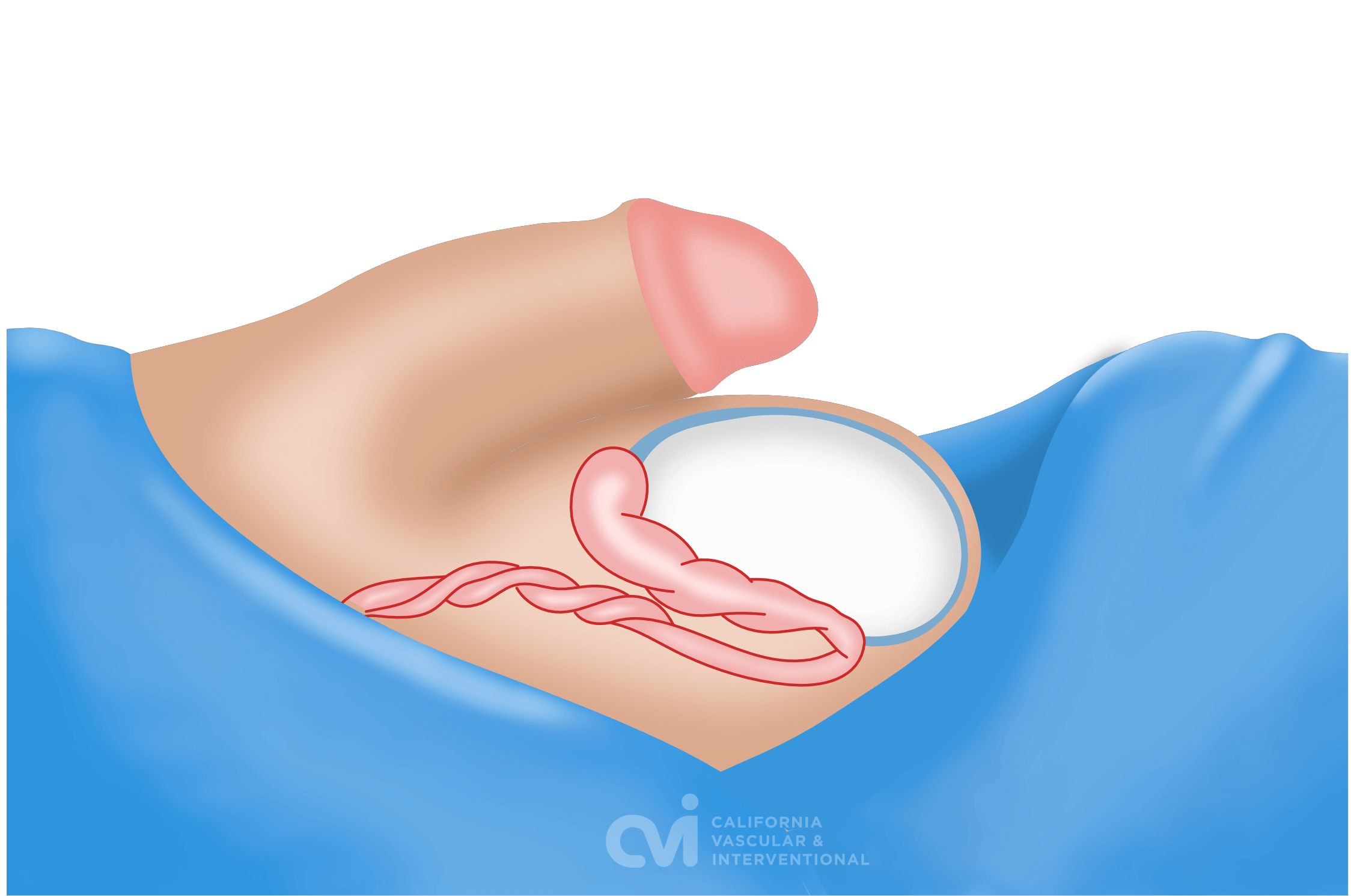
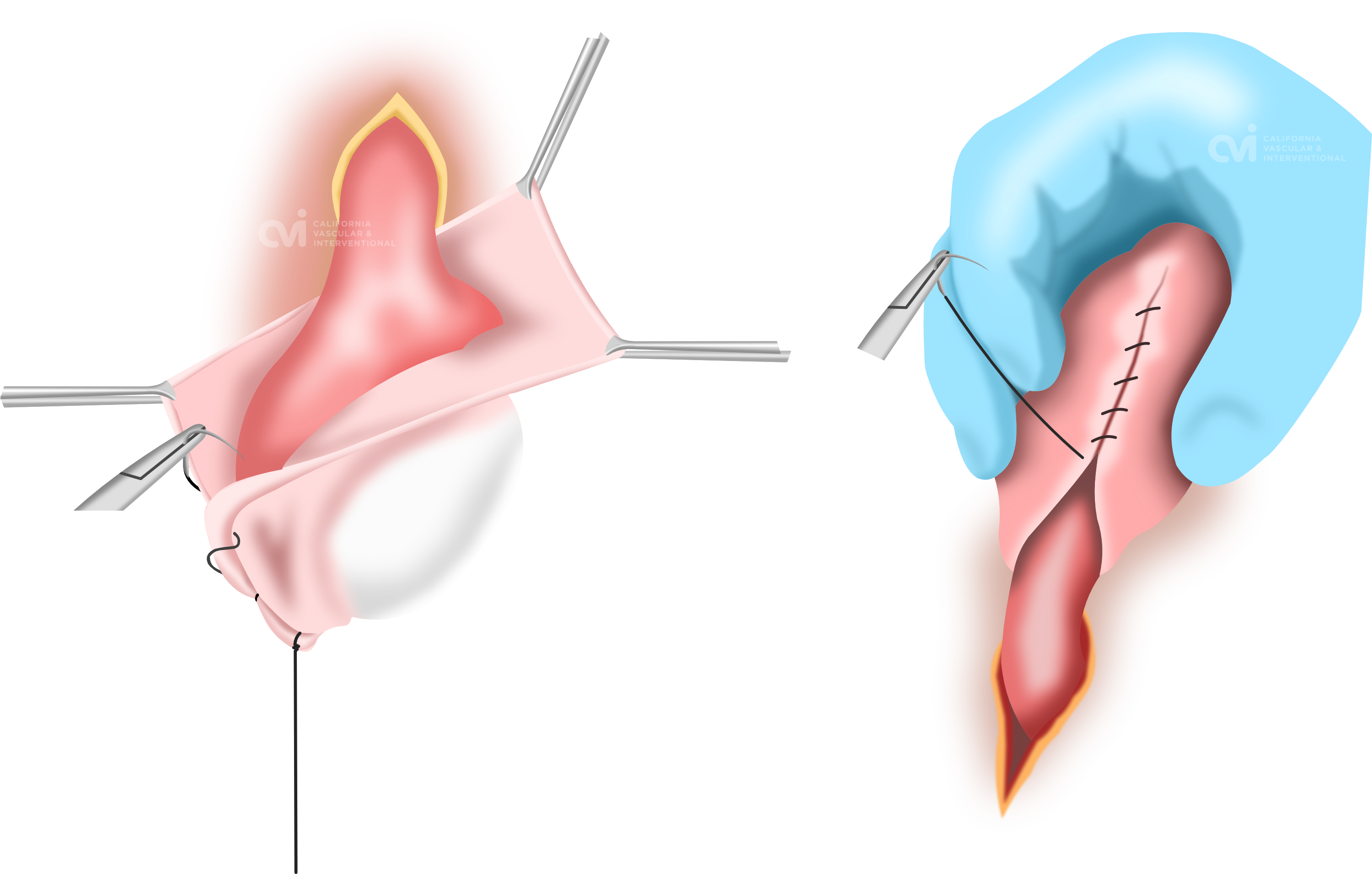
Surgical Excision or Spermatocelectomy
While we do not perform surgical removal of spermatocele you should understand and be informed of your surgical option. This procedure involves making an incision in your scrotum followed by dissection of the spermatocele without damaging surrounding epididymal tissue. The fluid and sac are then removed. The space is then sutured closed. After surgery, you need to wear an athletic support to protect the incision. You will also need pain medication and ice packs to keep the swelling down. Recovery from spermatocelectomy can take up to 5 days. Possible complications include continued pain, recurrence of the spermatocele, hematoma, and infection. Damage to the epididymis and/or vas deferens during the surgery can affect fertility. In one study, nearly 20% of patients who underwent surgical spermatocelectomy experienced postoperative complications such as treatment failure, chronic pain, and scrotal abscess formation. You can watch how spermatocele excision is performed via the following LINK: VIEWER'S DISCRETION ADVISED: GRAPHIC VIDEO (Please note we are not affiliated)
What is the right treatment for me?
If you’ve been diagnosed with a spermatocele it’s important to gain at least a basic understanding of your treatment options. Every approach to treatment has its pros and cons. Ultimately, the treatment you choose will depend on what your doctor recommends and what feels best to you. Some patients obtain surgery while others prefer a non-surgical option such as sclerotherapy, and only seek surgery if the treatment is not effective for them.
You should seek the expert advice of your urologist and our interventional radiologist to further understand your options and expected outcomes.
Our interventional specialist has performed more spermatocele sclerotherapy treatments than any other practitioner. In fact, most practitioners are unaware that such a treatment exists let alone to have experience in performing it. Spermatoceles tend to be much smaller than hydroceles and thus require a good understanding and experience with ultrasound. As such, we are the number one recommended and referred to practice for this treatment.
Over the years our specialist has developed his own technique based on experience on what works and what doesn't work. This has increased the success rates while decreasing the discomfort. Other practitioners have limited experience in this treatment and they typically perform aspirations blindly by jabbing a needle into the scrotum without ultrasound. One problem with this technique is that it almost always leave some fluid behind when the procedure is done blindly with a needle and without ultrasound guidance. If there is any residual fluid then the sclerotherapy does not work very well. This is just one of the many details that are important in having a successful outcome.
You can rest assured that your experience will be much more pleasant at CVI as the procedure is performed with precision using ultrasound guidance by our specialist. Our specialist has performed over 5,000 ultrasound guided procedures in addition to his experience in performing sclerotherapy injections.
Can't I just have aspiration to remove the spermatocele fluid?
Aspiration alone will not be sufficient. If your specialist only removes the fluid it will only be a matter of time that the spermatocele will return causing your symptoms again. Sclerotherapy is important as it closes the cavity, preventing the fluid from returning.
Our specialist performs the aspiration first using ultrasound-guidance. The ultrasound shows precisely the location of the needle so that the testicle or adjacent structures do not get punctured, essentially eliminating any risk thereof. Make sure that your specialist performing this procedure is trained in ultrasound-guided procedures.
My Urologist tried sclerotherapy and it didn't work. Is this the same?
No.
Most urologist will not offer aspiration and sclerotherapy. For urologists that do, they do not perform the procedure with the same technique as our specialist. There are several reasons why sclerotherapy by your urologist failed. The main reason is the lack of ultrasound guidance. Ultrasound confirms that all of the spermatocele fluid has been removed before injecting the medication. Any fluid left behind will dilute the medication rendering it inactive. Urologist perform this procedure blindly with a needle. There is no way to know if there is any fluid left in this manner. Needle aspiration is also not as effective in removing all of the fluid.
Our specialist performs the aspiration first using ultrasound-guidance. Ultrasound is used throughout the procedure to make sure the procedure is performed adequately and safely. The ultrasound shows precisely the location of the tube so that the testicle and adjacent structures do not get punctured, essentially eliminating any risks. Make sure that your specialist performing this procedure is trained in ultrasound-guided procedures. Our specialist performs more sclerotherapy treatments than any other specialist.
Our Patient Experiences
Sclerotherapy Cost
We do not accept insurance for sclerotherapy. Since the cost of the sclerotherapy is not covered by insurance, this is ideal for someone who feels strongly about avoiding surgery as there is an out of pocket cost. Please contact our office for the current charges.
Sclerotherapy is Not New
Sclerotherapy is not new! Sclerotherapy has been performed on fluid collections and cysts for decades! Our doctor performs sclerotherapy on large cysts in the liver, kidney and other structures for over 10 years. In other organs, our doctor leaves a drainage catheter and patients return for weekly sclerotherapy sessions until the cyst is gone. Due to the nature of the scrotum our doctor deploys a different method to achieve the same success without having to leave a catheter in place. Patient go home without a catheter, incision, suture or any bandaging.
Results
Sclerotherapy is a minimally-invasive, non-surgical, outpatient treatment for a scrotal spermatocele. It is quick, safe, and effective, and it avoids the expense and potential complications of surgery. There are no major incisions, no stitches, and no downtime. You can return to work immediately after the treatment.
The initial success rate of a single spermatocele aspiration and sclerotherapy procedure is more than 75%, meaning 3 out of 4 patients are symptom-free just after one treatment. With multiple treatments, the success rate improves to nearly 95%.
Appointments are available via an online video telehealth platform or in person at one of the offices in Los Angeles, Orange County or San Diego, depending on the doctor’s availability. Contact Us Today. Why should you choose us? Read here.
References:
1. Medscape: Spermatocele, updated Jan 02, 2019, Author: Vernon M Pais, Jr, MD.
2. Beiko DT, Morales A. Percutaneous aspiration and sclerotherapy for treatment of spermatoceles. J Urol. 2001 Jul;166(1):137-9. PMID: 11435841.
3. Kiddoo DA, Wollin TA, Mador DR. A population based assessment of complications following outpatient hydrocelectomy and spermatocelectomy. J Urol. 2004 Feb;171(2 Pt 1):746-8. doi: 10.1097/01.ju.0000103636.61790.43. PMID: 14713801.
4. Braslis KG, Moss DI. Long-term experience with sclerotherapy for treatment of epididymal cyst and hydrocele. Aust N Z J Surg. 1996 Apr;66(4):222-4. doi: 10.1111/j.1445-2197.1996.tb01169.x. PMID: 8611129.
The above information explains what is involved and the possible risks. It is not meant to be a substitute for informed discussion between you and your doctor, but can act as a starting point for such a discussion.
